The deaths of healthcare workers from the coronavirus are inevitable. That is how Nurse Sean Petty says he believes hospital and government leaders across the United States sees it.
“That makes us feel like our lives are expendable and we know that they are not,” says Petty, who works in the pediatric emergency room at Jacobi Hospital in the Bronx, New York.
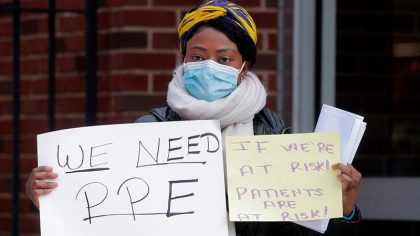
Petty and dozens of his fellow nurses protested outside the hospital earlier this week, pleading for more personal protective equipment (PPE) like masks, gloves and gowns.
Their demands have been echoed across the US, where health workers continue to grapple with the critical PPE shortages as the COVID-19 coronavirus hits towns, cities and states nationwide. More than 250,000 people have been infected with the virus in the US, with more than 5,000 deaths.
New York is the hardest hit, with more than 100,000 coronavirus cases and over 2,900 deaths.
Petty says that he and his fellow nurses are constantly exposed to the virus without enough PPE to protect themselves. His hospital lost a nurse, 50-year-old Freda Ocran, last week to COVID-19, the second nurse in New York to die from the virus. Two more nurses are currently being intubated at his hospital, according to Petty.
“We can’t help but think that being healthcare workers and not having what they had in other places, like what the PPE is like in China and South Korea … they’re just worlds apart,” Petty says.
Before Petty’s 12-hour shift begins, he reports to the new command centre set up outside his hospital to receive a packet containing a regular surgical mask, some paper scrubs and a light gown. Sometimes he gets a face mask. He also receives a new N95 mask for every shift and is expected to use the same one throughout the day.
Responding to the concerns of the nurses, NYC Health + Hospitals, which operates public hospitals and clinics in the city, said in a statement that the nurses’ safety is top priority.
“We currently have the supplies needed for all of our staff, but are fully cognizant that there is a nationwide shortage of supplies,” the statement said. “Because of the national picture, we have taken serious measures to conserve what we do have. However, every healthcare worker in our system who needs PPE is able to receive what they need.”
Elsewhere in the country, doctors and nurses are preparing for the onslaught of COVID-19 cases to hit their hospitals in the coming weeks.
Dr Susan George Knoche is a colorectal surgery specialist in Charleston, South Carolina, and has joined forces with other doctors, nurses and administrators at her hospital to start planning for possible PPE shortages and strategising how to best conserve what they have in stock. They have already ceased elective surgeries as one of the protective measures to conserve their limited PPE.
“We are so worried about the coming wave of COVID-19 that we have to sort of shut down operations as much as we can in preparation for it,” she says. “It’s like we’re sort of waiting standing there, like waiting with the doors open for the COVID-19 patients to start coming in,” Knoche adds.
Some doctors – like family practitioner Dr Sylvia Gisi in Temecula, California, who recently began testing her patients for the virus – say they have to go “underground” to get masks and goggles for her clinic, but the supplies are hard to find.
“This is the United States of America, this is not a third-world country, and yet the doctors and nurses and ancillary hospital staff are being treated like that,” she says about the lack of access to PPE.
The federal government’s emergency stockpile of PPE is nearly depleted, officials acknowledged this week. US media also reported that the US exported millions of dollars of PPE to China during the first two months of the year, despite expert warnings the coronavirus would soon spread to the US.
Even though the $2.2 trillion coronavirus stimulus package passed by Congress last month includes $117bn in aid for hospitals, doctors and nurses across the country still worry about their health systems collapsing.
“I’m afraid of that moment where we go from an incremental growth to a significant jump in volume in ill patients that we’re going to drown, and it’s going to be bad,” says Petty, the New York City nurse.

Freelanews is a potpourri of news, entertainment, business, events and photos. This is no fake news.